All published articles of this journal are available on ScienceDirect.
Multicultural Intensive Care: A Cross-sectional Study on Family-centered Care in the United Arab Emirates
Abstract
Introduction
Implementing Family-Centered Care (FCC) is widely recognized in healthcare settings for its quality and safety benefits. However, FCC in intensive care units (ICUs), particularly in highly diverse contexts such as the United Arab Emirates (UAE), poses additional challenges due to differing languages, religions, and cultural backgrounds. This cross-sectional study explores the dynamics of family and visitor interactions in UAE ICUs, aiming to provide insights that inform FCC implementation.
Objective
Understanding the core needs of families with relatives in ICUs is essential for the successful adoption of FCC, highlighting key factors required for effectively navigating the ICU environment.
Methods
From May to July 2024, a comprehensive study was conducted in selected critical care facilities across the UAE, involving approximately 240 adult family members closely associated with patients undergoing life-saving interventions. Data were gathered using the Critical Care Family Needs Inventory (CCFNI) Support Questionnaire. The data analysis was also conducted at the descriptive and inferential statistics level using SPSS version 16 software.
Results and Discussion
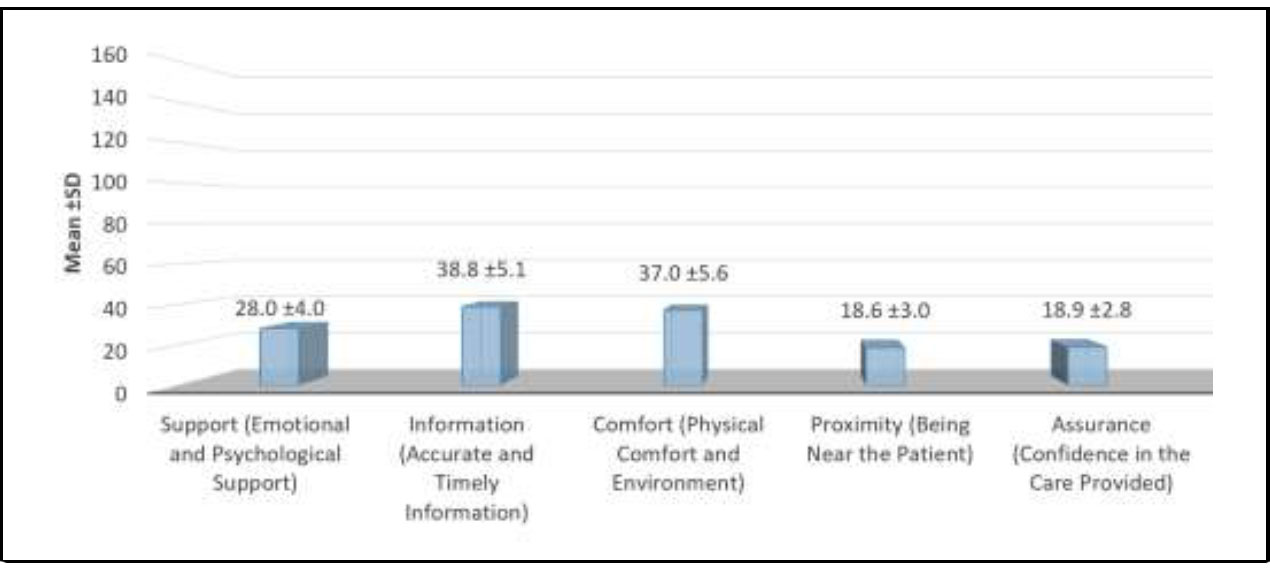
Among the five domains of the CCFNI, the highest mean score was for Information (38.8 ± 5.1), followed by Comfort (37.0 ± 5.6) and Support (28.0 ± 4.0). Proximity (18.6 ± 3.0) and Assurance (18.9 ± 2.8) recorded the lowest scores. Although families valued being near the patient and receiving assurance about care, their emotional support, timely information, and comfort needs remained insufficiently met in the UAE context.
Conclusion & Recommendations
Emotional support, timely information, and comfort should be prioritized to advance FCC in UAE ICUs. These findings can guide future research and foster the development of tailored support initiatives addressing the diverse needs of families. Also recommended to adapt visitation guidelines to allow increased family presence, particularly for critically ill patients, while maintaining infection control measures.
1. INTRODUCTION
During challenging times when a family member is admitted to an intensive care unit (ICU), the rest of the family often experiences significant stress and uncertainty. Their desire to provide support may be hampered by various factors, including insufficient information about the patient’s condition or how to assist, communication difficulties with healthcare professionals, and the emotional and psychological strain they face. In such circumstances, a lack of knowledge, reassurance, assistance, or support can leave family members feeling helpless, isolated, and insecure, thereby compromising the potential benefits they could provide [1-3].
In the United Arab Emirates (UAE), Arabic and Islamic cultures place a central emphasis on family involvement in healthcare, guided by religious, cultural, and ethical norms. Within the Islamic tradition, caring for an ill relative is deemed both a religious duty and an act of worship, underscoring the importance of family presence and assistance (Saifan et al., 2022) [4]. Families frequently make key healthcare decisions, particularly in critical or end-of-life situations, reflecting sociocultural values that uphold the well-being of the family unit. However, this robust family involvement may also cause practice complexity and ethical challenges regarding patient autonomy and the disclosure of medical information [5], resulting in hesitancy among healthcare professionals to fully adopt Family-Centered Care (FCC). Despite these obstacles, FCC inherently aligns with Islamic and Arabic principles by acknowledging the family’s pivotal role and their need for involvement in their patient's care [6, 7].
Although the UAE has seen a growing acceptance of FCC, its implementation faces additional complexities due to a diverse, multicultural population and reliance on expatriate healthcare providers [8]. While cultural diversity can enrich patient care, it can also introduce language barriers, unfamiliar customs, varied levels of acceptance of some concepts, varied commitment to care development, and disparate religious observances. Consequently, healthcare professionals require specialized training on FCC principles and local cultural norms, including Islamic values, to effectively meet patient and family expectations [8].
Equally important is assessing the needs and experiences of critically ill patients and their families, which is a critical component and the first foundational step of creating a more humanized ICU environment [1-3]. Critically ill patients frequently depend on family members to communicate their preferences and values. Active family participation in ICU settings significantly shapes a patient’s well-being [9-11]. Cagle and Bunting emphasize that families provide vital social and emotional support, contributing to holistic care [10-12]. Meeting these requirements can help reduce patient’s anxiety and cultivate familial trust in the healthcare system [13]. Failing to recognize family needs can lead to dissatisfaction and potentially diminish the quality of healthcare services [14]. Hence, addressing these needs is essential for maintaining patient and family satisfaction and optimizing health outcomes.
Globally, studies have shown that families of ICU patients prioritize different needs, ranging from effective communication to privacy or accommodation [15]. Hospital administrators and staff can enhance critical care outcomes by designing policies and initiatives tailored to the locally identified and prioritized needs of families [16]. Consequently, replicating such studies in the UAE context is vital to ensure that healthcare interventions resonate with the region’s unique cultural and societal nuances. Gaining an in-depth understanding of local family needs, challenges, and preferences will enable the development of culturally sensitive, contextually appropriate healthcare services [16].
1.1. Aim of the Study
This study aims to examine the core needs of families with relatives in intensive care within the culturally diverse context of the United Arab Emirates, identifying the key factors required for effectively implementing Family-Centered Care (FCC) and improving family engagement in the ICU setting.
1.2. Study Methods
1.2.1. Study Design
This study employed a quantitative, cross-sectional design, which involves collecting data to capture the immediate needs and experiences of families with relatives in intensive care. By surveying a diverse sample of participants from multicultural contexts, this approach offers an idea of family requirements, needs, and challenges within the ICU setting. These findings can then inform targeted strategies to improve Family-Centered Care (FCC) and guide future research.
1.2.2. Study Participants
Relatives of severely ill patients who are admitted to the CCUs that are involved in the study. The eligible family members must meet the following criteria: they must be at least eighteen years old, able to read and write in both Arabic and English, have a first-degree relationship with the patient, and have visited the patient within 48 to 72 hours after admission on at least two occasions.
1.2.3. Sample Size
Sample size was calculated based on the formula (Fisher formula, Cochran's formula) [17] ensuring a 95% confidence level and a 5% margin of error while estimating a 7% proportion in a large population. This calculation resulted in a required sample of approximately 240 family members. The anticipated response rate is 60%–80%, though non-responses may arise due to time constraints, emotional distress, or language barriers. To mitigate this, the study implements follow-up reminders, flexible survey formats, anonymity assurances, small incentives, and multilingual options. These strategies help maximize participation and minimize bias, ensuring a reliable and representative sample.
1.2.4. Study Setting
This study was carried out in adult Intensive Care Units (ICUs) located at hospitals in Dubai (one government hospital and one private hospital), Umm Al-Quwain (one government hospital and one private hospital), and Sharjah (two government hospitals and two private hospitals) and Ajman (one government hospital and one private hospital). These emirates are essential parts of the UAE's complex cultural fabric, including a wide range of habits, traditions, and history that reflect the greater community. It is essential to include these emirates in our study domain in order to fully understand the needs of families in critical care units. With a population that encompasses both urban centers and rural communities, they offer us the opportunity to document a wide array of experiences and preferences. This research aims to shed light on the variations in family demands in critical care settings among a culturally diverse and dynamic population by utilizing the unique characteristics of these emirates.
1.3. Data Collection Questionnaires
The Critical Care Family Needs Inventory (CCFNI) was derived from a study conducted by Leske in 1991 [18]. The study titled “The needs of family members of patients admitted to the intensive care unit,” is a reliable tool with a Cronbach's alpha score of 0.94. It is specifically designed to assess the perceived significance of different needs within the hospital setting. The tool is meticulously developed and consistently dependable and translated to Arabic version. The Critical Care Family Needs Inventory is composed of 45 need statements, typically grouped into the following areas:
• Support Questions (Emotional and Psychological Support) focus on emotional reassurance, understanding, and empathy from healthcare providers.
• Information Questions (Accurate and Timely Information) focus on regular updates about the patient’s condition and care plan.
• Comfort Questions (Physical Comfort and Environment) focus on the Physical needs of family members, such as a place to rest, food, or privacy.
• Proximity Questions (Being Near the Patient) focus on being physically close to the patient during critical care.
• Assurance Questions (Confidence in the Care Provided) focus on Trust and confidence in the healthcare team's competence.
Participants are required to assign a rating to each item, indicating its level of relevance, using a scale ranging from 1 to 4. The numerical scale used is as follows: 1 represents insignificance, 2 represents moderate significance, 3 represents significance, and 4 represents high significance. A strong Cronbach's alpha score enhances confidence in the scoring system and validates its capacity to precisely capture participants' opinions and priorities. The Patient and Family Needs Assessment Questionnaire has been enhanced in terms of its dependability and clearly defined framework, making it a helpful and trustworthy instrument for investigating the intricacies of patient and family experiences in healthcare environments.
1.4. Data Collection
Upon receipt and submission of the consent papers within a timeframe of one to three weeks, a package including questionnaires and a prepaid return envelope was dispatched by mail. The data was collected from May to July 2024.
The researcher visited the chosen CCUs to identify eligible family members. Members who met the requirements were requested to complete a questionnaire consisting of two sections. Family members were given a self-administered questionnaire during their break time in the day shift. They were required to sign an informed consent form before participating. The questionnaire took around 15 minutes to complete.
1.5. Ethical Consideration
The Ethics Review Board of the University of Sharjah has granted approval for the study under reference number: REC-22-02-07-04-S. In order to uphold ethical standards, the research was conducted in full adherence to the norms outlined in the Declaration of Helsinki [19].
A communication letter was sent out to tell potential participants and their families about the study which emphasized its voluntary nature, with the aim of engaging eligible individuals. The information packet included a well-informed consent form and a prepaid return envelope.
The study's findings ensured that all personal information would be anonymised and that the identity of the participants would remain undisclosed.
Furthermore, participants were granted the freedom to withdraw from the research at any point without being obligated to provide an explanation.
The data was securely handled and stored in compliance with statutory frameworks that govern data protection, research ethics, and research governance.
1.6. Data Analysis
The quantitative data for this study was meticulously analyzed using the SPSS software, specifically version 16.00 for Windows. In order to analyze the continuous variables in detail, the means and standard deviations (S.D.) of these variables were compared between the two groups. The researchers effectively assessed the numerical properties of the data through this approach. In addition, the One-way ANOVA test was employed to assess categorical data.
Through the use of statistical testing and ranking, a comprehensive examination was conducted to identify any disparities across various data points. The sorting of means and standard deviations enabled the identification of trends and variations in the continuous variables. However, the One-way ANOVA test revealed notable variations among the items in the category. By employing statistical techniques like linear regression, the research team conducted a comprehensive analysis of the data, examining all its dimensions and identifying any possible patterns or discrepancies among the groups.
2. RESULTS
Table 1 presents the distribution of socio-demographic characteristics of the study sample, consisting of 240 participants. The variables assessed include age, gender, relation with the patient, education level, and type of hospital.
| - | n | % |
|---|---|---|
| Age (Years) | - | - |
| < 30 | 68 | 28.3 |
| 30 – 39 | 67 | 27.9 |
| 40 – 49 | 53 | 22.1 |
| 50 – 59 | 52 | 21.7 |
| Mean ±SD | 38.5 ±12.3 | - |
| Gender | - | - |
| Male | 131 | 54.6 |
| Female | 109 | 45.4 |
| Relation with patient | - | - |
| Father / Mother | 26 | 10.8 |
| Brother / Sister | 50 | 20.8 |
| Son / Daughter | 148 | 61.7 |
| Uncle / Aunt | 16 | 6.7 |
| Education level | - | - |
| Basic | 20 | 8.3 |
| Preparatory | 17 | 7.1 |
| Secondary | 50 | 20.8 |
| Diploma | 41 | 17.1 |
| Bachelor | 112 | 46.7 |
| Type of hospital | - | - |
| Public | 151 | 62.9 |
| Private | 89 | 37.1 |
The age distribution of the participants shows the largest proportion (28.3%) of participants in the < 30 years age group. The 30-39 years group is the second largest, representing 27.9% of the sample. The 40-49 years and 50-59 years age groups represent 22.1% and 21.7% of the sample, respectively.
The sample size was more male-dominated, with 54.6% (131) of the participants being male and 45.4% (109) female. The largest group of participants (61.7%) were sons or daughters of the patient, highlighting their primary role as key decision-makers and caregivers in family-centered care, particularly in Middle Eastern and Islamic cultures, where children often assume responsibility for their aging or ill parents, followed by brothers or sisters which account for 20.8% of the participants. Fathers or mothers make up 10.8% of the respondents.
The highest proportion of participants (46.7%) have a Bachelor’s degree, and secondary education follows with 20.8% of respondents.
The majority of participants (62.9%) are associated with public hospitals, and a smaller portion (37.1%) are from private hospitals.
Table 2 presents the mean scores and standard deviations for the five key domains of the Critical Care Family Needs Inventory. These domains encompass emotional support, information, comfort, proximity, and assurance. Here are key observations and implications based on the scores:
The highest mean score is observed for Information (38.8), indicating that families prioritize accurate and timely information about their loved one's condition. This is followed closely by Comfort (37.0), suggesting that families also place considerable importance on the physical environment and their own comfort while in critical care settings. Support (28.0) is also valued but to a slightly lesser extent, indicating that emotional and psychological support is important but may be considered secondary to information and comfort. The domains of Proximity (18.6) and Assurance (18.9) are rated the lowest, suggesting that while they matter, they are less of a priority for families compared to the other needs.
| - | Mean ±SD |
|---|---|
| Critical Care Family Needs Inventory domains | - |
| Support (Emotional and Psychological Support) | 28.0 ±4.0 |
| Information (Accurate and Timely Information) | 38.8 ±5.1 |
| Comfort (Physical Comfort and Environment) | 37.0 ±5.6 |
| Proximity (Being Near the Patient) | 18.6 ±3.0 |
| Assurance (Confidence in the Care Provided) | 18.9 ±2.8 |
| Critical Care Family Needs Inventory total score | 141.4 ±18.8 |
Fig. (1) provides an assessment of the five domains of the Critical Care Family Needs Inventory. The highest mean score is in the Information domain (38.8 ± 5.1), followed by Comfort (37.0 ± 5.6) and Support (28.0 ± 4.0). The Proximity (18.6 ± 3.0) and Assurance (18.9 ± 2.8) domains have the lowest mean scores. Overall, the total score of 141.4 ± 18.8 reflects the cumulative importance of these domains, with a relatively high level of perceived need for emotional and informational support in the critical care setting.
Table 3 emphasizes the critical need for emotional and psychological support among families in intensive care settings. A vast majority prioritize knowing the expected outcome (99.2%) and receiving honest answers to their questions (69.6% very important). While visitation rights are valued, only 17.9% rate them as very important. Support from friends (78.3%) and understanding the roles of medical staff (82.9%) are also significant concerns. Additionally, families express a need for a private space in the hospital, though responses are mixed, with 42.9% considering it important. Financial support emerges as a major concern, with 90% of respondents rating it as important or very important. Emotional expression, such as feeling comfortable while crying, is also valued by 69.6% of families. Lastly, access to family support services is deemed necessary by 74.2% of participants. Overall, these findings highlight the importance of clear communication, financial assistance, and emotional well-being for families navigating the ICU experience.
Table 4 highlights the information needs of families in critical care settings, emphasizing the importance of clear communication and guidance. Families prioritize understanding the ICU environment before entering (83.8%) and expect flexibility in visiting hours for special circumstances (90.5%). Many express a need to discuss their emotions (82.6%) and receive guidance on bedside behavior (85%). Hope is a crucial factor, with 90.5% considering it important or very important. Families also value assurance of quality care (93.8%) and detailed updates on medical procedures (90.9%). While pastoral visits are less prioritized (63.4%), discussions about patient mortality (77.5%) and reassurance about leaving the hospital (77.9%) hold significance. Additionally, families emphasize timely visiting hours (86.2%) and expect regular patient updates (93.7%). These findings underscore the critical role of consistent, transparent, and empathetic communication in supporting families during their loved ones' ICU stay.
Assessment of the critical care family needs inventory domains and total score.
| - | Not Important | Slightly Important | Important | Very Important | |||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||
| Support (Emotional and Psychological Support) | - | - | - | - | - | - | - | - | |
| To know the expected outcome | 2 | 0.8 | 0 | 0.0 | 78 | 32.5 | 160 | 66.7 | |
| To have questions answered honestly | 0 | 0.0 | 2 | 0.8 | 71 | 29.6 | 167 | 69.6 | |
| To visit at any time | 45 | 18.8 | 40 | 16.7 | 112 | 46.7 | 43 | 17.9 | |
| To have friends nearby for support | 5 | 2.1 | 47 | 19.6 | 115 | 47.9 | 73 | 30.4 | |
| To know about the types of staff members taking care of the patient | 4 | 1.7 | 37 | 15.4 | 109 | 45.4 | 90 | 37.5 | |
| To have a place to be alone while in the hospital | 29 | 12.1 | 65 | 27.1 | 103 | 42.9 | 43 | 17.9 | |
| To have someone to help with financial problems | 4 | 1.7 | 20 | 8.3 | 92 | 38.3 | 124 | 51.7 | |
| To feel it is alright to cry | 22 | 9.2 | 51 | 21.3 | 112 | 46.7 | 55 | 22.9 | |
| To be told about someone to help with family problems | 21 | 8.8 | 41 | 17.1 | 131 | 54.6 | 47 | 19.6 | |
| - | Not Important | Slightly Important | Important | Very Important | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| Information (Accurate and Timely Information) | - | - | - | - | - | - | - | - |
| To have explanations of the environment before going into the critical care unit for the first time | 12 | 5.0 | 27 | 11.3 | 84 | 35.0 | 117 | 48.8 |
| To have visiting hours changed for special conditions | 3 | 1.3 | 20 | 8.3 | 99 | 41.3 | 118 | 49.2 |
| To talk about feelings about what has happened | 6 | 2.5 | 36 | 15.0 | 99 | 41.3 | 99 | 41.3 |
| To have directions as to what to do at the bedside | 3 | 1.3 | 33 | 13.8 | 114 | 47.5 | 90 | 37.5 |
| To feel there is hope | 5 | 2.1 | 18 | 7.5 | 82 | 34.2 | 135 | 56.3 |
| To be assured that the best care possible is being given to the patient | 0 | 0.0 | 15 | 6.3 | 63 | 26.3 | 162 | 67.5 |
| To know exactly what is being done for the patient | 5 | 2.1 | 17 | 7.1 | 94 | 39.2 | 124 | 51.7 |
| To have a pastor visit | 18 | 7.5 | 70 | 29.2 | 107 | 44.6 | 45 | 18.8 |
| To talk about the possibility of the patient's death | 27 | 11.3 | 27 | 11.3 | 110 | 45.8 | 76 | 31.7 |
| To be assured it is alright to leave the hospital for awhile | 27 | 11.3 | 26 | 10.8 | 109 | 45.4 | 78 | 32.5 |
| To have visiting hours start on time | 7 | 2.9 | 26 | 10.8 | 127 | 52.9 | 80 | 33.3 |
| To receive information about the patient at least once a day | 5 | 2.1 | 10 | 4.2 | 110 | 45.8 | 115 | 47.9 |
| - | Not Important | Slightly Important | Important | Very Important | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| Comfort (Physical Comfort and Environment) | - | - | - | - | - | - | - | - |
| To talk to the doctor every day | 4 | 1.7 | 20 | 8.3 | 104 | 43.3 | 112 | 46.7 |
| To have a specific person to call at the hospital when unable to visit | 8 | 3.3 | 13 | 5.4 | 105 | 43.8 | 114 | 47.5 |
| To have good food available in the hospital | 33 | 13.8 | 45 | 18.8 | 83 | 34.6 | 79 | 32.9 |
| To know which staff members could give what type of information | 7 | 2.9 | 17 | 7.1 | 111 | 46.3 | 105 | 43.8 |
| To know why things were done for the patient | 6 | 2.5 | 13 | 5.4 | 82 | 34.2 | 139 | 57.9 |
| To have comfortable furniture in the waiting room | 30 | 12.5 | 64 | 26.7 | 86 | 35.8 | 60 | 25.0 |
| To have another person with you when visiting the critical care unit | 23 | 9.6 | 70 | 29.2 | 90 | 37.5 | 57 | 23.8 |
| To talk to the same nurse every day | 35 | 14.6 | 56 | 23.3 | 105 | 43.8 | 44 | 18.3 |
| To have a bathroom near the waiting room | 20 | 8.3 | 48 | 20.0 | 111 | 46.3 | 61 | 25.4 |
| To help with the patient's physical care | 10 | 4.2 | 11 | 4.6 | 90 | 37.5 | 129 | 53.8 |
| To feel that the hospital personnel care about the patient | 2 | 0.8 | 10 | 4.2 | 119 | 49.6 | 109 | 45.4 |
| To have the waiting room near the patient | 17 | 7.1 | 59 | 24.6 | 108 | 45.0 | 56 | 23.3 |
Table 5 highlights the physical comfort and environmental needs of families in a critical care setting. Families highly value daily communication with doctors (90%) and a designated contact person at the hospital (91.3%). Understanding staff roles and medical decisions is crucial, with 90.1% wanting clarity on procedures. While good hospital food is important (67.5%), 13.8% find it unnecessary. Comfort in waiting areas receives mixed responses, with furniture (60.8%) and nearby bathrooms (71.7%) seen as moderately important. Support during visits (66.7%) and consistent nurse interaction (62.1%) hold significance, though not top priorities. Family involvement in patient care (91.3%) and feeling hospital staff genuinely care (95%) are among the most valued aspects. Additionally, the proximity of waiting rooms to patients is important for 68.3%. These insights reinforce the importance of clear communication, emotional reassurance, and practical accommodations for families navigating critical care environments.
Table 6 highlights the proximity-related needs of families in critical care settings. The most crucial need is understanding the patient’s medical treatment, with 92.9% rating it as important or very important. Feeling accepted by hospital staff is also significant (89.6%), followed by having someone concerned about their health (65.4%). While being alone at times is moderately important (57.1%), it is not a priority for most. Information about chaplain services is valued by 79.2%, and being informed about transfer plans is a top concern, with 93.4% rating it highly. These findings emphasize the importance of clear communication, emotional support, and transparency in critical care environments.
Table 7 outlines the assurance-related needs of families in critical care. The most critical concerns include being called about changes in the patient's condition (95.8% rated it as important or very important) and receiving understandable explanations (92.9%). Families also prioritize knowing specific facts about the patient’s progress (97.1%) and seeing the patient frequently (88.8%). While learning about other sources of help is valued (70.0%), having a telephone near the waiting room is less critical, with only 56.3% considering it important or very important. These results underscore the need for clear communication, timely updates, and frequent access to loved ones in critical care settings.
Table 8 explores the association between socio-demographic characteristics (age, gender, relation with the patient, education level, and type of hospital) and the Critical Care Family Needs Inventory domains and total score. The table presents the mean scores for five domains (Support, Information, Comfort, Proximity, and Assurance) based on socio-demographic groups, along with statistical analyses (ANOVA and Student’s t-test). Here’s an interpretation of the findings:
Age emerged as a significant factor in determining families’ needs, with older participants (40–49 years) reporting higher requirements across most domains, particularly for information, comfort, proximity, and assurance. By contrast, gender did not show statistically significant differences in any of the domains (p > 0.05). Similarly, the participant’s relationship with the patient whether as a parent, sibling, child, or aunt/uncle—did not influence reported needs (p > 0.05). Education level, however, played a notable role: those holding a Bachelor’s degree consistently indicated higher needs across all domains. In addition, the type of hospital (public vs. private) significantly affected the Proximity domain (T=2.188, P=0.030), with families in public hospitals expressing a slightly greater need (18.9) to remain near their loved one than those in private hospitals (18.1).
| - | Not Important | Slightly Important | Important | Very Important | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| Proximity (Being near the patient) | - | - | - | - | - | - | - | - |
| To know how the patient is being treated medically | 2 | 0.8 | 15 | 6.3 | 89 | 37.1 | 134 | 55.8 |
| To feel accepted by the hospital staff | 4 | 1.7 | 21 | 8.8 | 116 | 48.3 | 99 | 41.3 |
| To have someone be concerned with your health | 38 | 15.8 | 45 | 18.8 | 89 | 37.1 | 68 | 28.3 |
| To be alone at any time | 29 | 12.1 | 74 | 30.8 | 108 | 45.0 | 29 | 12.1 |
| To be told about chaplain services | 9 | 3.8 | 41 | 17.1 | 127 | 52.9 | 63 | 26.3 |
| To be told about transfer plans while they are being made | 5 | 2.1 | 11 | 4.6 | 87 | 36.3 | 137 | 57.1 |
| - | Not Important | Slightly Important | Important | Very Important | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| Assurance (Confidence in the care provided) | - | - | - | - | - | - | - | - |
| To have a telephone near the waiting room | 38 | 15.8 | 67 | 27.9 | 76 | 31.7 | 59 | 24.6 |
| To be told about other people that could help with problems | 24 | 10.0 | 48 | 20.0 | 121 | 50.4 | 47 | 19.6 |
| To have explanations given that are understandable | 5 | 2.1 | 12 | 5.0 | 100 | 41.7 | 123 | 51.2 |
| To be called at home about changes in the patient's condition | 4 | 1.7 | 6 | 2.5 | 98 | 40.8 | 132 | 55.0 |
| To know specific facts concerning the patient's progress | 0 | 0.0 | 7 | 2.9 | 125 | 52.1 | 108 | 45.0 |
| To see the patient frequently | 9 | 3.8 | 18 | 7.5 | 137 | 57.1 | 76 | 31.7 |
| - | Support | Information | Comfort | Proximity | Assurance | Critical Care Family Needs Inventory total score |
|---|---|---|---|---|---|---|
| Mean ±SD | Mean ±SD | Mean ±SD | Mean ±SD | Mean ±SD | Mean ±SD | |
| Age (Years) | - | - | - | - | - | - |
| < 30 | 28.7 ±4.1 | 39.3 ±4.4 | 38.2 ±6.0 | 19.1 ±2.8 | 19.5 ±2.6 | 144.9 ±18.0 |
| 30 – 39 | 27.0 ±4.6 | 37.3 ±6.3 | 35.1 ±6.1 | 18.1 ±3.6 | 18.2 ±3.6 | 135.7 ±23.1 |
| 40 – 49 | 29.6 ±3.2 | 40.7 ±4.8 | 39.3 ±4.7 | 19.7 ±2.5 | 20.0 ±2.6 | 149.2 ±16.3 |
| 50 – 59 | 26.6 ±3.0 | 38.3 ±3.4 | 35.7 ±3.6 | 17.5 ±2.1 | 18.1 ±1.3 | 136.2 ±11.0 |
| Oneway ANOVA | F=7.387, p<0.001** | F=5.148, P=0.002* | F=8.299, p<0.001** | F=6.388, p<0.001** | F=7.106, p<0.001** | F=7.840, p<0.001** |
| Gender | - | - | - | - | - | - |
| Male | 27.6 ±3.5 | 39.1 ±4.4 | 36.6 ±4.7 | 18.7 ±2.6 | 19.0 ±2.5 | 141.1 ±15.8 |
| Female | 28.4 ±4.5 | 38.4 ±5.8 | 37.5 ±6.4 | 18.6 ±3.3 | 18.9 ±3.1 | 141.8 ±21.9 |
| Student’s t – test | T=1.400, P=0.163 | T=1.074, P=0.284 | T=1.235, P=0.218 | T=0.203, P=0.839 | T=0.189, P=0.850 | T=0.313, P=0.755 |
| Relation with patient | - | - | - | - | - | - |
| Father / Mother | 27.2 ±3.6 | 38.2 ±4.3 | 35.9 ±4.7 | 17.8 ±2.5 | 18.4 ±2.4 | 137.5 ±16.6 |
| Brother / Sister | 28.2 ±3.6 | 39.3 ±3.9 | 36.5 ±4.4 | 18.8 ±2.2 | 18.7 ±2.6 | 141.5 ±14.6 |
| Son / Daughter | 27.8 ±4.3 | 39.0 ±5.5 | 37.4 ±6.2 | 18.6 ±3.3 | 19.2 ±3.0 | 142.1 ±21.0 |
| Uncle / Aunt | 29.9 ±2.1 | 36.8 ±5.0 | 37.0 ±2.9 | 19.4 ±2.2 | 17.9 ±.8 | 140.9 ±11.3 |
| Oneway ANOVA | F=1.721, P=0.163 | F=1.232, P=0.299 | F=0.695, P=0.556 | F=1.119, P=0.342 | F=1.809, P=0.146 | F=0.445, P=0.721 |
| Education level | - | - | - | - | - | - |
| Basic | 23.7 ±3.9 | 35.6 ±3.6 | 35.1 ±2.6 | 16.9 ±1.4 | 16.6 ±0.8 | 127.9 ±10.9 |
| Preparatory | 27.8 ±4.4 | 38.2 ±6.1 | 36.4 ±5.5 | 18.8 ±2.9 | 19.4 ±3.1 | 140.6 ±21.1 |
| Secondary | 28.2 ±3.3 | 38.7 ±4.2 | 37.4 ±5.6 | 18.4 ±2.4 | 19.2 ±2.3 | 142.0 ±15.5 |
| Diploma | 29.1 ±3.6 | 40.5 ±4.6 | 37.5 ±5.2 | 18.7 ±3.3 | 19.2 ±2.9 | 144.9 ±18.3 |
| Bachler | 30.7 ±4.4 | 41.4 ±5.6 | 39.6 ±6.1 | 20.6 ±3.3 | 20.7 ±3.1 | 153.1 ±21.1 |
| Oneway ANOVA | F=18.153, p<0.001** | F=7.365, p<0.001** | F=4.171, P=0.003* | F=10.146, p<0.001** | F=10.438, p<0.001** | F=9.449, p<0.001** |
| Type of hospital | - | - | - | - | - | - |
| Public | 28.4 ±4.4 | 38.9 ±5.6 | 37.2 ±6.0 | 18.9 ±3.2 | 19.1 ±2.9 | 142.4 ±20.8 |
| Private | 27.3 ±3.1 | 38.8 ±4.1 | 36.8 ±4.8 | 18.1 ±2.5 | 18.7 ±2.6 | 139.7 ±14.9 |
| Student’s t – test | T=1.913, P=0.057 | T=0.143, P=0.887 | T=0.464, P=0.643 | T=2.188, P=0.030* | T=0.915, P=0.361 | T=1.061, P=0.290 |
3. DISCUSSION
This study provides a critical foundation for the advancement of Family-Centered Care (FCC) in critical care units (CCUs) within the United Arab Emirates (UAE). By identifying the needs of families with relatives in intensive care, these findings offer clear direction for initiatives that are more focused, organized, and ultimately more likely to succeed. Meeting these needs is not only essential for minimizing the psychological stress families face but also crucial for tapping into their ability to contribute positively to patient care and outcomes. A CCU encompasses both intensive care units (ICUs) and high-dependency units (HDUs)—settings where families commonly experience tension, anxiety, and sadness [20]. In the UAE, male family members often serve as the main caregivers and hospital companions, in contrast to the cultural norms of other regions where women typically fulfill this role [21-25]. This difference underscores the importance of tailoring FCC strategies to local cultural contexts and ensuring that they align with the roles that family members naturally assume.
The current findings highlight the specific ways in which family needs in the UAE diverge from international norms, such as emphasizing the importance of accurate information and suitable physical amenities like lodging. These observations align with previous research indicating that when information needs remain unmet, families may feel overlooked or poorly utilized in the care process [21, 26-28]. Conversely, when they receive sufficient support and timely updates, families can become active partners in care, ultimately improving patient outcomes. Participants strongly voiced a desire for clear communication regarding the health status of their critically ill relatives and the procedures being performed. Related studies [26, 27] confirm that families experience additional distress when the diagnosis, prognosis, and plan of care are insufficiently explained and that comprehensive information-sharing can empower families to act effectively as patient advocates [28, 29]. Another significant area of concern in this study was the provision of physical resources. Consistent with Hsieh et al. [30], families emphasized the need for comfortable waiting areas, adequate nutrition, and rest, particularly since many travel from distant regions to access specialized facilities. Meeting these environmental needs can lessen stress and improve the overall experience for both families and patients.
Strong psychosocial needs also emerged, encompassing emotional support, reassurance, and close proximity to the patient. High levels of worry, stress, or sadness are common in CCUs [20, 22, 31, 32], and addressing these emotional burdens through open communication, empathy, and psychological services can help both families and patients cope more effectively. Being able to identify healthcare professionals—by having staff wear clear identification—was highlighted as a simple but impactful step to reduce confusion and anxiety [29]. Families also viewed proximity as an integral aspect of care monitoring. Extended or more flexible visiting hours could allow families to stay closer to their relatives, which not only reduces their anxiety but also enhances their trust in the care provided [20-35].
Public hospital families, in particular, reported higher needs for proximity, suggesting that policies limiting visiting times should be revisited to accommodate these needs. Sociodemographic factors further influenced family perspectives: older participants (40–49 years) registered greater needs for information, comfort, proximity, and assurance, possibly reflecting a combination of increased life experience and more active roles within the family. Meanwhile, families with higher education were more likely to demand detailed information and supportive measures, aligning with Bandari et al. [27], who argue that education fosters greater awareness of critical care processes and the desire for increased involvement.
CONCLUSION
This study highlights the critical role of the FCC in meeting the diverse needs of families in multicultural ICU settings in the UAE. While proximity and assurance were valued, significant gaps remained in emotional support, timely information, and comfort. Addressing these unmet needs through enhanced communication, culturally sensitive support services, and flexible visitation policies can improve family experiences and contribute to better patient outcomes. Implementing tailored FCC strategies will be essential in fostering a more inclusive and supportive ICU environment.
LIMITATIONS
Although this study’s sample size was sufficient for the quantitative surveys conducted at multiple hospitals, the representation of participants from specific facilities and localities may limit the applicability of findings to all regions of the United Arab Emirates. Family needs could vary across different cultural and geographic contexts, and a more extensive, regionally diverse sample in future research would provide a more comprehensive understanding of family requirements throughout the UAE.
AUTHORS’ CONTRIBUTIONS
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| UAE | = United Arab Emirates |
| FCC | = Family-centered Care |
| ICUs | = Intensive Care Units |
| CCFNI | = Critical Care Family Needs Inventory |
| S.D. | = Standard Deviations |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethical approval was obtained from the Ethics Review Board of the University of Sharjah, UAE under Reference number: REC-22-02-07-04-S.
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
A communication letter was sent out to tell potential participants and their families about the study and emphasize its voluntary nature, with the aim of engaging eligible individuals. The information packet included a well-informed consent form and a prepaid return envelope.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article will be available from the corresponding author [M.N.] upon reasonable request.
ACKNOWLEDGEMENTS
Declared none.